Tumour tissues as part of the biological sample collection around the world become part of the Mutographs project following strict eligibility criteria, based on pathology examination. This process is part of work package 1 (WP1), led by Paul Brennan and centralised in the International Agency for Research in Cancer (IARC) in France.
Behnoush Abedi-Ardekani (MD) a scientist and pathologist at IARC takes us through the meticulous analysis of Mutographs tissue samples to determine their suitability for sequencing and further analysis at the Wellcome Sanger Institute, UK.
What is pathology and why it is part of Mutographs?
Pathology is a medical specialty which means “studying lesions”. Every disease in our body is caused by the accumulation of toxic factors that eventually affect the integrity and functionality of our cells and their genomic content, leading to symptoms and signs. Clinical symptoms appear when pathological structural and cellular changes have already been established in our body. The ultimate aim of all physicians is the correct diagnosis of disease and appropriate planning for patient management. The pathologists’ aim is the same, with a deeper level of analysis: “studying and interpreting cellular changes at microscopic level”. The pathologist adds this level of information to clinical and radiological data to provide a final diagnosis. The discovery of the microscope in the 19th century led to a revolutionary change to the field of pathology from studying gross pathologies to cellular levels. Today, impressive advances in technology and whole genome sequencing, have shifted the understanding of diseases to the genomic level. Equally, modern pathology is not limited to analysis of cellular and morphological features, but greatly expanded to the analysis, interpretation and integration of these features with molecular data. Molecular pathology is a new era of practice in the field.
Cancer is a chronic disease and pathology has a crucial role in diagnosis, morphological and molecular typing, and guidance of the therapeutic approaches and patient management. The principal role of pathology is the same in both diagnosis and research. While genomic analysis lies at the base of the Mutographs project, pathology is the fundamental part of the process that serves to evaluate the cancer tissues and to confirm their characteristics and suitability for the study.
Pathology workflow of Mutographs samples at IARC
Mutographs aims to analyse the genomic data of 5000 cancers, from five cancer types. Around 40 collaborating centers distributed in five continents are recruiting patients and collecting their biological material, including a piece of cancer tissue. The collected tissues are preserved frozen, stored in local centers and shipped to IARC in appropriate and regular timetables for microscopic examination and extraction of genomic content (DNA) of eligible ones. In a medical set up, we don’t freeze tissues for the purpose of diagnosis, but research needs go further than microscopy alone and we know that the genomic content of cells is better preserved when frozen. As a result, the Mutographs’ tissue samples must be examined frozen, which is much more challenging for the pathologist than the routine practice of analysing fixed tissues.
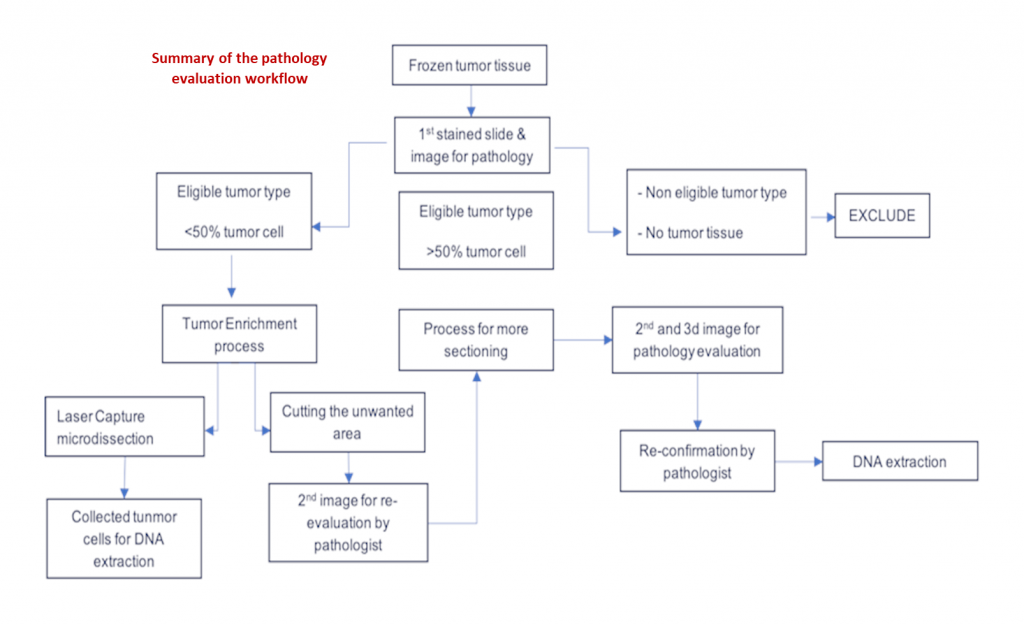
Let’s follow the journey of Mutographs’s biological material, specifically the cancer tissues, through their processing and evaluation at IARC:
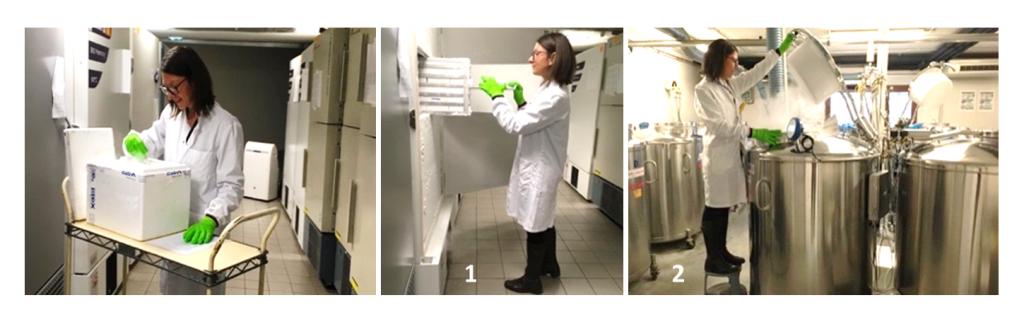
Priscilia, a laboratory research assistant, receives all biological material, performs quality control, and transfers it to a -80º C freezer (1) or a liquid nitrogen container (2).
When the biological material arrives at IARC, it is transferred to deep-freezing storage.

Christine, a pathology research assistant, sections blocks of frozen tissues (1) in a cryostat (2).
Then the tissues are gradually taken to the pathology lab, where they are prepared for analysis. The frozen tissues are sectioned by cryostat: a sharp blade in a cold chamber at -30°C. The ultrathin sections 3μm thick are placed on labelled glass slides. The remaining tissue is kept in a frozen block and are stored back in the freezer.
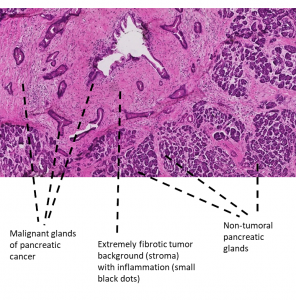
In order to visualise the details of the ultrathin sections of tissue on the slides, they need to be stained. The routine and first level staining for all tissues is called H&E and consists of Hematoxylin and Eosin that create a contrast between cellular components. Hematoxylin stains the nuclei blue and Eosin stains tha cytoplasm of the cells and the extracellular matrix of tissues pink. The intensity of the colours, the ratio between them and their distribution in the tissue provides valuable information, vital for pathologists to provide a diagnosis.
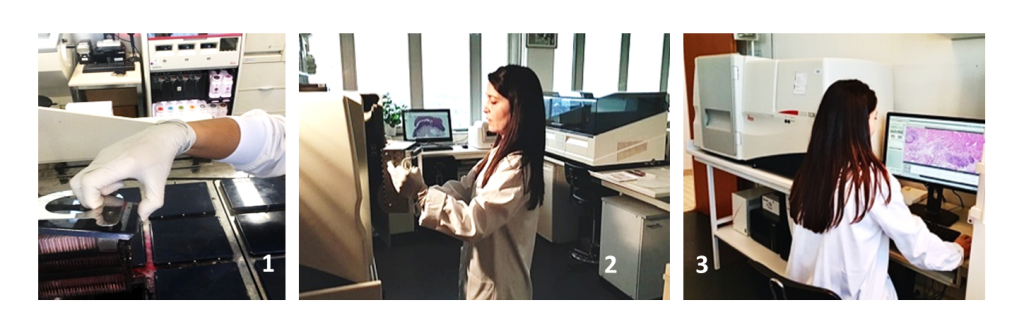
Christine stains the sections (1), scans them through a Leica digital scanner and transforms them to digital images (2). Finally, she checks the quality of the images before releasing them to the pathologist (3).
Behnoush, the leader of the pathology workflow, examines some of the cases and distributes a fraction of the the images to the external pathologists.
The high quality images are then analysed in fine detail by a team of pathologists with specific expertise. The Mutographs pathology workflow is led by Bahnoush Abedi-Ardekani. She oversees the entire process and provides microscopic reports of the tissues in collaboration with a team of eight external pathologists: six gastrointestinal pathologists and two nephropathologists. Each cancer tissue sample is examined and reported by one pathologist and a randomly selected 20% of samples are independently examined and reported by two experts. Every pathologist has the option of consulting for a second opinion through the web-based pathology report platform. Any disagreement between the analyses is resolved by seeking a third report or a re-examination and discussion session.
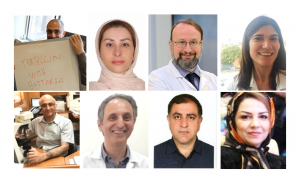
External expert pathology team, left to right: Stefano, Hiva, Jean-Yves, Sophie, Masoud, Farid, Arash and Mojgan.

Independent pathology reports are provided using image-based digital pathology and a web-based pathology report platform.

Valérie, the senior data manger, extracts the reports and selects the eligible cases to build the list of approved tissues.
The samples with a confirmed morphological type with at least 50% viable cells are selected and a list is sent to the biobank.

Christophe, the senior biobank assistant, performs automated DNA extraction of the listed samples.
Finally, those samples containing at least 800 ng of DNA are kept and the DNA shipped to the Wellcome Sanger Institute in the UK for whole genome sequencing and analysis. Pathology examination and genomics complement each other to drive forward cancer research.